Abstract
Introduction: Myelofibrosis (MF), either primary or secondary, belongs to Philadelphia-negative myeloproliferative neoplasms (MPN) and is characterized by bone marrow fibrosis, hematopoietic stem cell mobilization and extramedullary hematopoiesis. Compelling evidence are suggesting that persistent antigen stimulation in the tumor microenvironment can differentiate T effector cells into terminally exhausted T cells, a functional state characterized by decrease in proliferation, cytotoxicity, and cytokine production. Innovative therapies aim at reversing the exhausted state through immune checkpoint inhibition to recover the immune response against the tumor. Even in myeloid neoplasms such as MPNs, T cells are showing dysfunctional features; thus we investigated T cell exhaustion in MF to assess the possibility of immune checkpoint inhibition as a new effective therapy.
Methods: Peripheral blood mononuclear cells (PBMCs) were isolated from 44 MF patients and 22 healthy donors (HD). CD3+CD8+ T cells were characterized by multicolor flowcytometry to assess surface expression of the following inhibitory receptors (IRs): PD-1, CD244, CD160, TIM-3, LAG-3, CTLA-4. Results were correlated with clinical features such as Dynamic International Prognostic Scoring System (DIPSS) classification, splenomegaly, high-molecular risk (HMR) mutation number and other negative prognostic factors. We performed intracellular flowcytometry staining to assess residual cytokine production in PBMCs stimulated overnight with anti-CD3, anti-CD28 and Brefeldin A. Total cellular RNA was isolated from granulocytes of 141 primary and secondary MF patients and 28 HDs, and we performed Gene expression profiling (GEPs) by microarray platform to evaluate IRs-ligands expression. To test the possible inhibitory effect of the neoplastic clone we cultured T cells either alone or in co-culture with the myeloid cells for 4 days in the presence of anti-CD3/CD28 stimulatory beads, SCF, TPO, FLT3l, IL6, IL7 and IL15 and then we tested the activation marker OX40 expression level. The co-culture system was also used to test the effect of CTLA-4 inhibition.
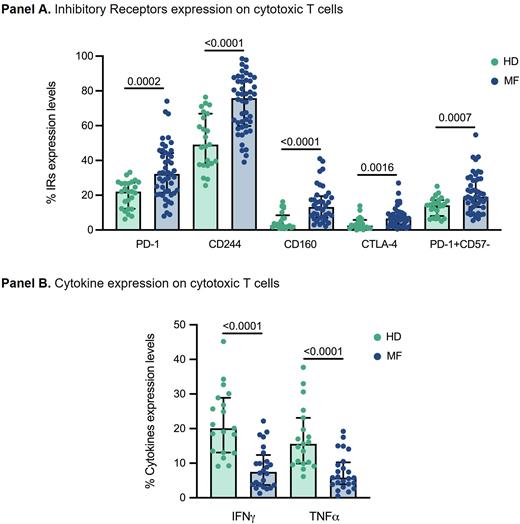
Results: We observed increased expressions of PD-1, CD244, CTLA-4 and CD160 on cytotoxic T cells from MF patients together with the expansion of PD-1+CD57- cytotoxic T cell populations (Panel A), which also showed increased expression of all the IRs assessed, with CD160 and CTLA-4 being the more significantly upregulated. Higher levels of PD-1, CD244, CD160, CTLA-4, LAG-3 or TIM-3 on cytotoxic T cells correlate with detrimental features like splenomegaly, low hemoglobin levels, HMR mutation number and more severe DIPSS classification. Moreover, we observed decreased secretion of IFNɣ and TNFɑ by total CD3+CD8+ T cells and PD1+ subpopulation from MF patients (Panel B). A significant reduction of Granzyme B production was observed mainly in patients with expansion of PD1+CD57- exhausted T cells. GEPs analysis highlighted increased expression of IR-ligands like CD274, CEACAM1, CD48, CD80 on granulocytes from MF patients compared to HDs. While cytotoxic T cells from HDs were effectively activated either alone or in co-culture with myeloid cells, the activation of cytotoxic T cells from MF patients was damped in presence of myeloid cells and restored when T cells were cultured alone. Treatment with anti-CTLA-4 was able to partially restore the MF T cells activation potential in the presence of myeloid cells.
Conclusions: Our data evidenced in MF patients the presence of an impaired population of peripheral blood cytotoxic T cells expressing multiple IRs and with reduced cytokine production after in vitro activation. Clinical correlations suggest a more severe disease in patients with higher IRs expression on cytotoxic T cells. Moreover, granulocytes from MF patients display higher level of IR-ligands transcripts suggesting an immunosuppressive interplay between the myeloid neoplastic clone and T cells. This was also suggested by reduced activation level of T cells in co-culture with myeloid cells that was restored by removing of myeloid cells or with anti-CTLA-4 treatment. Taken together this data highlights an exhausted state likely implicated in immune escape that could be targeted and potentially reverted by immune checkpoint inhibitions.
Disclosures
Mora:Novartis: Speakers Bureau. Guglielmelli:Novartis, Abbvie: Other: Other member of advisory board, speaker at meeting. Passamonti:BMS: Research Funding; Novartis, Celgene, BMS, Abbvie, Janssen, Roche, AOP Orphan, Karyopharma, KYOWA KIRIN, Mei: Consultancy, Honoraria, Speakers Bureau. Luppi:Abbvie, Jazz Pharma, Gilead sci, MSD, Novartis, Sanofi, Daiichi-Sankyo, Grifols: Membership on an entity's Board of Directors or advisory committees; Gilead sci: Other: Travel grant. Vannucchi:Morphosys: Membership on an entity's Board of Directors or advisory committees; AOP Orphans Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Abbvie: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees; BluePrint: Membership on an entity's Board of Directors or advisory committees, Other: NA; BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees; GSK: Membership on an entity's Board of Directors or advisory committees, Other: NA; Incyte: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal